By Olivier Varenne, PI of the trial
The CAOCT study is an investigator-initiated trial held thanks to a grant from Abbott Vascular and consists of a prospective, multi-centre, single cohort, diagnostic accuracy study. The study aims to compare the angio to the OCT to evaluate the ability to detect the culprit lesion. 131 patients, survivors of OHCA will be included in France, Serbia and Belgium. The trial is undergoing regulatory review.
Out-of-hospital cardiac arrest (OHCA) is a leading cause of sudden death in Europe and the United States. Mortality is currently close to 40% among those patients who had been successfully resuscitated after OHCA associated with ventricular fibrillation or pulseless ventricular tachycardia. Coronary artery disease is observed in up to 70% of patients with OHCA and immediate coronary angiography. Current European and American guidelines recommend immediate coronary angiography with primary angioplasty in OHCA patients with ST-segment elevation on ECG after successful resuscitation. However, in patients with OHCA but without ST-segment elevation on ECG after return of spontaneous circulation (ROSC), systematic immediate coronary angiography has not been shown to improve 90-day survival when compared to delayed angiography. Moreover, detection of significant coronary artery disease in survivors of an OHCA does not necessarily translate into a causal link to explain cardiac arrest. Furthermore, the identification of the culprit lesion by coronary angiography among patients with an acute coronary syndrome (ACS) and no OHCA is challenging.
In the Coronary Angiography after cardiac arrest (COACT) trial, a randomized controlled trial comparing immediate versus delayed coronary angiography after OHCA in patients without ST segment elevation on ECG, some degree of coronary artery disease was found in 64.5% of the patients in the immediate angiography group and an unstable coronary lesion was identified in only 13.6% of the patients. However, in survivors of OHCA without ST segment elevation on ECG, the use of intra coronary optical computerized tomography (OCT) led to identification of plaque rupture (27%), plaque erosion (36%) and coronary thrombosis (59%) undetected on angiography in a pilot study.
There is hence a clear need to improve causality diagnosis among patients resuscitated after OHCA and without ST segment elevation on ECG, and, in the case of coronary artery disease detection, to better identify the culprit vessel/lesion ultimately leading to a targeted treatment. These are the reasons why we have designed a prospective, multi-centre, single cohort, diagnostic accuracy study: to better explore the incidence of a true ACS among OHCA survivors and to evaluate the accuracy of angiography to detect the culprit lesion when compared to OCT.
The principal objective of the study is to evaluate the value of Optical Coherence Tomography (OCT) core lab analysis compared to coronary angiography core lab analysis, to detect a culprit unstable coronary lesion triggering out-of hospital cardiac arrest (OHCA) in patients without ST-segment elevation after return of spontaneous circulation (ROSC) ECG.
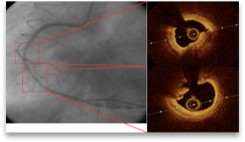
Figure. 55- y-old male after OHCA. ECG showed no ST elevation.
Left panel: non significant lesion is observed in first lesion with more severe distally.
Right panel : Severe atheroma is revealed by OCT without plaque rupture/erosion or thrombus on the first lesion. The distal lesion of the RCA is more severe with plaque rupture and thrombus.
